The importance of infection control in dentistry
2025-06-23 13:28:48

The importance of infection control in dentistry
The importance of infection control in dental practice cannot be overstated, especially given the critical nature of the procedures involved and the potential risks associated with exposure to pathogens. Dental environments are unique in that they involve close contact with patients, often in settings where blood and saliva are present. Therefore, stringent infection control measures are vital not only for patient safety but also for the protection of dental healthcare workers and the community at large. Here’s a summary of the key points regarding sterilization and disinfection practices in dentistry, along with additional insights and considerations.
Key Points on Infection Control in Dentistry
-
Sterilization of Critical Items:
-
Instruments that penetrate skin or mucosa (e.g., needles, surgical knives) must be either heat-sterilized or disposed of after use. The use of autoclaves is standard practice in many dental offices, ensuring that instruments are subjected to high-pressure steam, which effectively kills all forms of microbial life.
-
Handpieces, despite not penetrating mucosa, are classified as critical items and require heat sterilization. Regular maintenance and cleaning protocols for handpieces are also essential to prevent biofilm formation, which can harbor bacteria.
-
Semicritical Items:
-
Items that come into contact with mucosa or non-intact skin (e.g., intraoral film holders) should also be heat-sterilized to ensure safety. For items that cannot withstand heat, chemical disinfection methods must be employed, following manufacturer guidelines to ensure efficacy.
-
It is crucial to implement a systematic approach to managing semicritical items, including proper labeling and storage after sterilization to avoid cross-contamination.
-
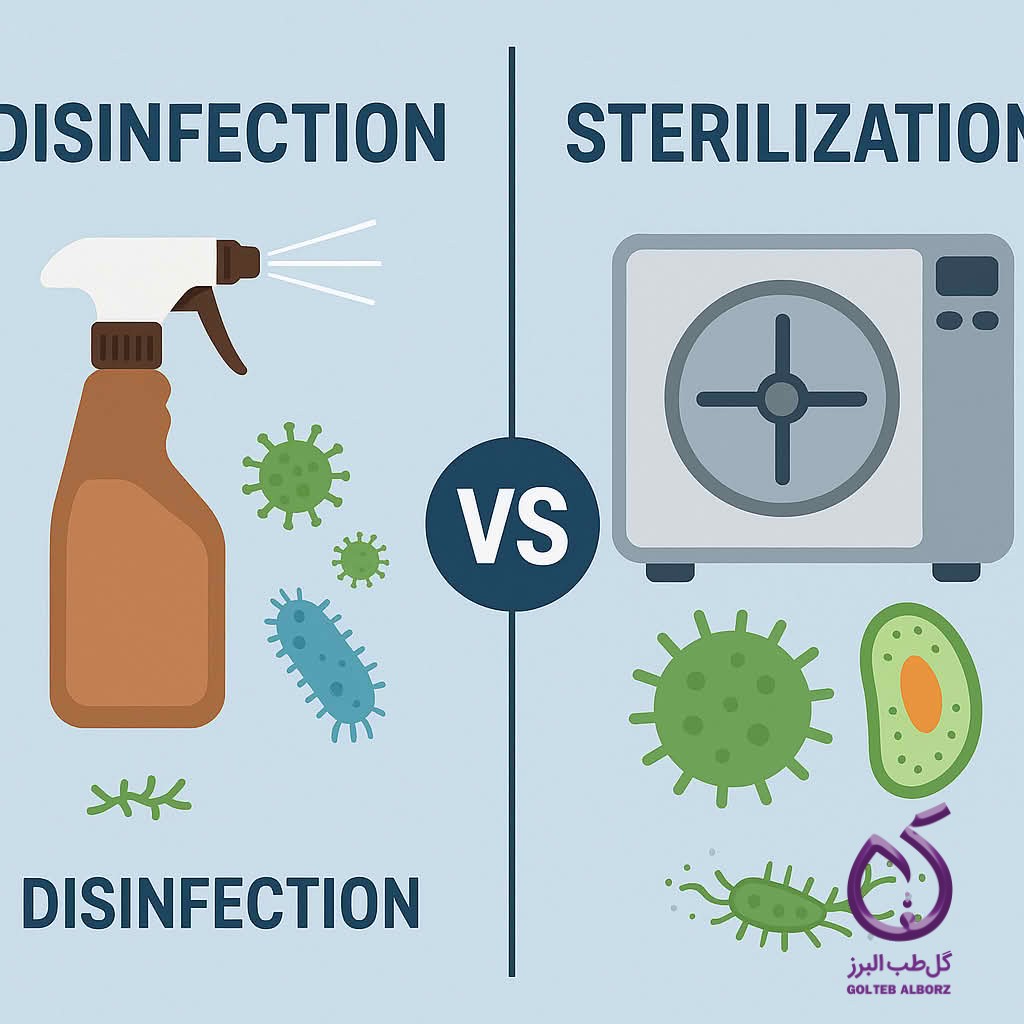
Disinfection vs. Sterilization:
-
Disinfection: This process eliminates most harmful microorganisms from surfaces and inanimate objects but does not guarantee the destruction of all pathogens. High-level disinfection is necessary for certain items that cannot be sterilized, and dental practices should utilize EPA-registered disinfectants that are effective against a broad spectrum of pathogens.
-
Sterilization: This process ensures that all microorganisms, including resistant bacterial spores, are killed, providing a higher level of safety. Regular biological monitoring of sterilization processes is recommended to verify that sterilizers are functioning correctly.
-
Ongoing Vigilance:
-
Infection control practices in dentistry have evolved significantly over the past two decades due to emerging threats such as airborne diseases (e.g., tuberculosis) and new infections like COVID-19. The pandemic highlighted the need for enhanced protocols, including the use of personal protective equipment (PPE) such as masks, face shields, and gowns to minimize exposure risk.
-
Dental health care workers must stay informed about the latest developments in infection control to protect both their patients and themselves. This includes participating in continuing education courses and staying updated on guidelines from reputable organizations such as the Centers for Disease Control and Prevention (CDC) and the American Dental Association (ADA).
-
Patient Education:
-
Educating patients about infection control measures can foster trust and enhance their understanding of the importance of these practices. Informing patients about what to expect during their visits and how their safety is prioritized can alleviate anxiety and encourage compliance with pre-appointment protocols, such as screening for symptoms.
-
Environmental Controls:
-
The dental office environment itself plays a crucial role in infection control. Regular cleaning and disinfection of surfaces, along with proper ventilation systems, can significantly reduce the risk of pathogen transmission. Implementing routine environmental assessments can help identify areas needing improvement.
-
Emerging Technologies:
-
Advances in technology, such as the use of ultraviolet (UV) light for disinfection and advanced air filtration systems, are becoming more prevalent in dental practices. These technologies can complement traditional methods and offer additional layers of protection against infectious agents.

Conclusion
Maintaining rigorous infection control protocols is essential for dental practitioners. By understanding the differences between disinfection and sterilization, adhering to established guidelines for critical and semicritical items, and embracing new technologies and practices, dental professionals can help mitigate risks and ensure a safe environment for patient care. Continuous education, adaptation to new challenges, and proactive patient engagement will further enhance public health safety in dental settings. Ultimately, the commitment to infection control is not just a regulatory requirement; it is a fundamental aspect of ethical dental practice that prioritizes the health and well-being of both patients and practitioners alike.
subscribe to newsletter
Find out about our latest discounts and news
Latest Articles
04
August
Understanding MID: How It Relates to Pulpotomy and Pulp Capping
Read more
28
July
Speed Up Tooth Socket Healing with Ora-Aid Oral Dressings
Read more
27
July
Bioceramic Materials in Pediatric Dentistry
Read more
15
July
Ora-Aid oral adhesive – overview & benefits video
Read more